TOOLS AND RESOURCES
Download the following tools and resources for detailed information about ARCALYST and how to use it:

ARCALYST Brochure

DOCTOR DISCUSSION GUIDE

ARCALYST STEP-BY-STEP INJECTION MANUAL

ARCALYST STEP-BY-STEP INJECTION VIDEO

Injection Tracker Manual
tips for ongoing success
Everybody's journey with recurrent pericarditis and ARCALYST is different. However, here are some tips for success that people with recurrent pericarditis and their doctors have shared:
Keep a journal.
Track how you are feeling between appointments as well as any questions you have for your doctor.
Build trust with your doctors.
They are part of your team and can provide answers and support beyond your prescription. Be honest with them about your expectations, hesitations, and goals throughout this process.
Speak up for yourself.
Your perspective is important, and your doctor needs to know what you are thinking and feeling in order to help you. Don’t be afraid to ask any and all questions you may have and get a second opinion if you feel you need one.
Lean on your support system.
Share what you are going through with the people in your life so they can understand how you are doing and how recurrent pericarditis impacts you. Ask them for help and support when you need it.
Stay in touch with your Patient Access Lead (PAL).
They will continue to check in with you while you are taking ARCALYST. Lean on them for support by asking questions and letting them help you.
Frequently asked questions
These FAQs are here to provide valuable information about ARCALYST and recurrent pericarditis.
Be sure to discuss your treatment options with your doctor and to contact the Kiniksa OneConnect™ program at 1-833-KINIKSA (1-833-546-4572) for additional information and support.
ARCALYST is a prescription medicine called an interleukin-1 (IL-1) blocker.
- ARCALYST is used to treat adults and children 12 years and older with Cryopyrin-Associated Periodic Syndromes (CAPS), including Familial Cold Autoinflammatory Syndrome (FCAS), and Muckle-Wells Syndrome (MWS)
- ARCALYST is used to maintain control of symptoms of Deficiency of Interleukin-1 Receptor Antagonist (DIRA) in adults and children weighing at least 22 pounds (10 kg)
- ARCALYST is used to treat Recurrent Pericarditis (RP) and reduce the risk of recurrence in adults and children 12 years and older
It is not known if ARCALYST is safe and effective in children under 12 years of age. It is not known if ARCALYST is safe and effective in children with DIRA weighing less than 22 pounds (10 kg).
To find a doctor who may be able to treat your recurrent pericarditis, a great place to start is with your insurance provider. Visit their website to view the doctors in your network. In many circumstances, insurance plans will not only list doctors and their specialties, but also list the conditions they treat. Additionally, there are patient advocacy groups such as the Pericarditis Alliance, Myocarditis Foundation, and American Heart Association that may provide support and resources.
Before starting treatment with ARCALYST, tell your healthcare provider if you:
- Think you have an infection
- Are being treated for an infection
- Have signs of an infection, such as fever, cough, or flu-like symptoms
- Have any open sores on your body
- Have a history of infections that keep coming back
- Have asthma. People with asthma may have an increased risk of infection
- Have diabetes or an immune system problem. People with these problems have a higher chance for infections
- Have tuberculosis (TB), or if you have been in close contact with someone who has had tuberculosis
- Have or have had HIV, hepatitis B, or hepatitis C
- Take other medicines that affect your immune system
Before you begin treatment with ARCALYST, talk with your healthcare provider about your vaccine history. Ask your healthcare provider whether you should receive any vaccines, including the pneumonia vaccine and flu vaccine, before you begin treatment with ARCALYST.
ARCALYST can affect your immune system. ARCALYST can lower the ability of your immune system to fight infections. Serious infections, including life-threatening infections and death, have happened in people taking ARCALYST. Taking ARCALYST can make you more likely to get infections, including life-threatening serious infections, or may make any infection that you have worse.
You should not begin treatment with ARCALYST if you have an infection or have infections that keep coming back (chronic infection).
After starting ARCALYST, if you get an infection, any sign of an infection, including a fever, cough, flu-like symptoms, or have any open sores on your body, call the healthcare provider right away. Treatment with ARCALYST should be stopped if you get a serious infection.
You should not take medicines that block tumor necrosis factor (TNF), such as Enbrel® (etanercept), Humira® (adalimumab), or Remicade® (infliximab), while you are taking ARCALYST. You should also not take other medicines that block interleukin-1 (IL-1), such as Kineret® (anakinra), while taking ARCALYST. Taking ARCALYST with any of these medicines may increase your risk of getting a serious infection.
Before starting treatment with ARCALYST, tell the healthcare provider if you:
- Think you have an infection
- Are being treated for an infection
- Have signs of an infection, such as fever, cough, or flu-like symptoms
- Have any open sores on your body
- Have a history of infections that keep coming back
- Have asthma. People with asthma may have an increased risk of infection
- Have diabetes or an immune system problem. People with these problems have a higher chance for infections
- Have tuberculosis (TB), or if you have been in close contact with someone who has had tuberculosis
- Have or have had HIV, hepatitis B, or hepatitis C
- Take other medicines that affect your immune system
Before you begin treatment with ARCALYST, talk with the healthcare provider about your vaccine history. Ask the healthcare provider whether you should receive any vaccines, including the pneumonia vaccine and flu vaccine, before you begin treatment with ARCALYST.
See Prescribing Information for additional safety information for ARCALYST
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially tell your healthcare provider if you take other medicines that affect your immune system, such as medicines that block tumor necrosis factor, interleukin-1, or corticosteroids.
You should not take medicines that block tumor necrosis factor (TNF), such as Enbrel® (etanercept), Humira® (adalimumab), or Remicade® (infliximab), while you are taking ARCALYST. You should also not take other medicines that block interleukin-1 (IL-1), such as Kineret® (anakinra), while taking ARCALYST. Taking ARCALYST with any of these medicines may increase your risk of getting a serious infection.
You should not receive live vaccines if you take ARCALYST.
Tell your healthcare provider if you are pregnant or plan to become pregnant:
- It is not known if ARCALYST will harm your unborn child. Tell your healthcare provider right away if you become pregnant while taking ARCALYST
- If you are breastfeeding or plan to breastfeed. It is not known if ARCALYST passes into breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with ARCALYST
ARCALYST can cause serious side effects, including:
Serious side effects:
- Serious Infections. ARCALYST can affect your immune system. ARCALYST can lower the ability of your immune system to fight infections. Serious infections, including life-threatening infections and death, have happened in people taking ARCALYST. Taking ARCALYST can make you more likely to get infections, including life-threatening serious infections, or may make any infection that you have worse.
- Risk of Cancer. Medicines that affect the immune system may increase the risk of getting cancer.
- Allergic Reaction. Stop taking or giving ARCALYST and call the healthcare provider or get emergency care right away if you get any of the following symptoms of an allergic reaction while taking ARCALYST:
- Rash
- Swollen face
- Trouble breathing
- Changes in your blood cholesterol and triglycerides (lipids). Your healthcare provider will do blood tests to check for these changes.
Common side effects:
- In people with CAPS and RP, the most common side effects of ARCALYST include:
- Injection-site reactions including: pain, redness, swelling, itching, bruising, lumps, inflammation, skin rash, blisters, warmth, and bleeding at the injection site.
- Upper respiratory tract infections
- Joint and muscle aches in RP
- In people with DIRA, the most common side effects of ARCALYST include:
- Upper respiratory tract infections
- Rash
- Ear infection
- Sore throat
- Runny nose
These are not all the possible side effects of ARCALYST. Tell your healthcare provider if you have any side effect that bothers you or does not go away. For more information, ask your healthcare provider or pharmacist.
The Kiniksa OneConnect™ program is made up of a team of dedicated Patient Access Leads who provide personalized one-on-one support at each step of your treatment journey with ARCALYST. You can find services to help you with starting treatment, financial assistance, and treatment support. You can contact a Kiniksa OneConnect™ team member at 1-833-KINIKSA (1-833-546-4572) Monday-Friday (8 AM – 8 PM ET).
Your Kiniksa OneConnect™ Patient Access Lead will help you coordinate the delivery of your medication and supplies.
ARCALYST Clinical Educators are qualified personnel who can assist you with virtual or in-person training to help you better understand the self-injection process.
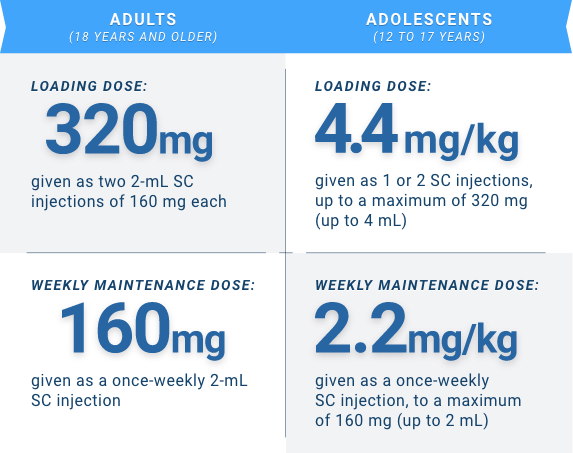
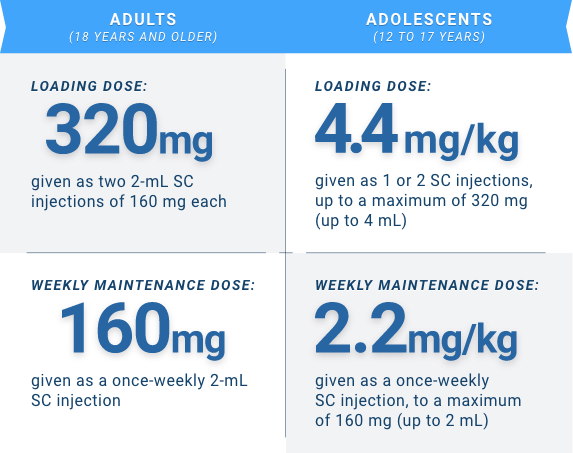
Your first dose of ARCALYST (referred to as the loading dose) will be given as 2 injections of ARCALYST with the help of a healthcare provider in their office or with support from an ARCALYST Clinical Educator.
The loading dose is twice the dose of the following, once-weekly “maintenance doses” that you will prepare and self-administer.
SC, subcutaneous.
Take ARCALYST exactly as prescribed by your healthcare provider.
ARCALYST is given by injection under the skin (subcutaneous injection) 1 time each week. A healthcare provider will tell you how much ARCALYST to take. The Kiniksa OneConnect™ program can work with you to set up one-on-one injection training sessions with an ARCALYST Clinical Educator, so you are familiar with the administration process. Do not try to give yourself ARCALYST injections until you are sure that you understand how to prepare and inject your dose. Call your healthcare provider, pharmacist, or your Kiniksa OneConnect™ Patient Access Lead at 1-833-KINIKSA (1-833-546-4572) if you have any questions.
Other resources include the Step-by-Step Injection video, the Step-by-Step Injection manual and the ARCALYST Instructions for Use.
ARCALYST is a once-weekly, self-administered medication given by injection under the skin (subcutaneous).
Keep ARCALYST in the carton it comes in to protect it from light. Store ARCALYST in the refrigerator between 36 °F and 46 °F (2 °C and 8 °C). Refrigerated ARCALYST can be used until the expiration date printed on the vial and carton. ARCALYST may be kept at room temperature after mixing with sterile water for injection and should be used within 3 hours of mixing.
Keep ARCALYST away from light, and keep ARCALYST, injection supplies, and all other medicines out of the reach of children.
If you miss a dose, you should speak with your healthcare provider.
For more information, please see the full Prescribing Information.
It is normal for the powder in the ARCALYST vial to appear as a solid clump or disc. If this is observed, continue following the steps related to the reconstitution of ARCALYST as outlined in the Instructions for Use. You may need to shake the vial back and forth for an extended period of time (repeat step 25 in the Instructions for Use) until the powder has completely dissolved and the solution is clear.
ARCALYST should be stored in the refrigerator between 36 °F and 46 °F (2 °C and 8 °C) until it is time to prepare the product for your dose.
If you receive your ARCALYST and the product feels warm to the touch or the temperature monitor inside the shipping container has been activated, please contact your Patient Access Lead who can provide guidance on the use of the product.
Talk to your healthcare provider if you experience any side effects that bother you or that do not go away. Please report side effects by contacting Kiniksa Pharmaceuticals toll-free at 1-833-546-4572, Option 3, or contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Active ingredient: rilonacept.
Inactive ingredients: glycine, histidine, L-arginine, polyethylene glycol 3350, and sucrose.
ARCALYST is a prescription medicine called an interleukin-1 (IL-1) blocker.
- ARCALYST is used to treat adults and children 12 years and older with Cryopyrin-Associated Periodic Syndromes (CAPS), including Familial Cold Autoinflammatory Syndrome (FCAS), and Muckle-Wells Syndrome (MWS)
- ARCALYST is used to maintain control of symptoms of Deficiency of Interleukin-1 Receptor Antagonist (DIRA) in adults and children weighing at least 22 pounds (10 kg)
- ARCALYST is used to treat Recurrent Pericarditis (RP) and reduce the risk of recurrence in adults and children 12 years and older
It is not known if ARCALYST is safe and effective in children under 12 years of age. It is not known if ARCALYST is safe and effective in children with DIRA weighing less than 22 pounds (10 kg).
To find a doctor who may be able to treat your recurrent pericarditis, a great place to start is with your insurance provider. Visit their website to view the doctors in your network. In many circumstances, insurance plans will not only list doctors and their specialties, but also list the conditions they treat. Additionally, there are patient advocacy groups such as the Pericarditis Alliance, Myocarditis Foundation, and American Heart Association that may provide support and resources.
Before starting treatment with ARCALYST, tell your healthcare provider if you:
- Think you have an infection
- Are being treated for an infection
- Have signs of an infection, such as fever, cough, or flu-like symptoms
- Have any open sores on your body
- Have a history of infections that keep coming back
- Have asthma. People with asthma may have an increased risk of infection
- Have diabetes or an immune system problem. People with these problems have a higher chance for infections
- Have tuberculosis (TB), or if you have been in close contact with someone who has had tuberculosis
- Have or have had HIV, hepatitis B, or hepatitis C
- Take other medicines that affect your immune system
Before you begin treatment with ARCALYST, talk with your healthcare provider about your vaccine history. Ask your healthcare provider whether you should receive any vaccines, including the pneumonia vaccine and flu vaccine, before you begin treatment with ARCALYST.
ARCALYST can affect your immune system. ARCALYST can lower the ability of your immune system to fight infections. Serious infections, including life-threatening infections and death, have happened in people taking ARCALYST. Taking ARCALYST can make you more likely to get infections, including life-threatening serious infections, or may make any infection that you have worse.
You should not begin treatment with ARCALYST if you have an infection or have infections that keep coming back (chronic infection).
After starting ARCALYST, if you get an infection, any sign of an infection, including a fever, cough, flu-like symptoms, or have any open sores on your body, call the healthcare provider right away. Treatment with ARCALYST should be stopped if you get a serious infection.
You should not take medicines that block tumor necrosis factor (TNF), such as Enbrel® (etanercept), Humira® (adalimumab), or Remicade® (infliximab), while you are taking ARCALYST. You should also not take other medicines that block interleukin-1 (IL-1), such as Kineret® (anakinra), while taking ARCALYST. Taking ARCALYST with any of these medicines may increase your risk of getting a serious infection.
Before starting treatment with ARCALYST, tell the healthcare provider if you:
- Think you have an infection
- Are being treated for an infection
- Have signs of an infection, such as fever, cough, or flu-like symptoms
- Have any open sores on your body
- Have a history of infections that keep coming back
- Have asthma. People with asthma may have an increased risk of infection
- Have diabetes or an immune system problem. People with these problems have a higher chance for infections
- Have tuberculosis (TB), or if you have been in close contact with someone who has had tuberculosis
- Have or have had HIV, hepatitis B, or hepatitis C
- Take other medicines that affect your immune system
Before you begin treatment with ARCALYST, talk with the healthcare provider about your vaccine history. Ask the healthcare provider whether you should receive any vaccines, including the pneumonia vaccine and flu vaccine, before you begin treatment with ARCALYST.
See Prescribing Information for additional safety information for ARCALYST
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially tell your healthcare provider if you take other medicines that affect your immune system, such as medicines that block tumor necrosis factor, interleukin-1, or corticosteroids.
You should not take medicines that block tumor necrosis factor (TNF), such as Enbrel® (etanercept), Humira® (adalimumab), or Remicade® (infliximab), while you are taking ARCALYST. You should also not take other medicines that block interleukin-1 (IL-1), such as Kineret® (anakinra), while taking ARCALYST. Taking ARCALYST with any of these medicines may increase your risk of getting a serious infection.
You should not receive live vaccines if you take ARCALYST.
Tell your healthcare provider if you are pregnant or plan to become pregnant:
- It is not known if ARCALYST will harm your unborn child. Tell your healthcare provider right away if you become pregnant while taking ARCALYST
- If you are breastfeeding or plan to breastfeed. It is not known if ARCALYST passes into breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with ARCALYST
ARCALYST can cause serious side effects, including:
Serious side effects:
- Serious Infections. ARCALYST can affect your immune system. ARCALYST can lower the ability of your immune system to fight infections. Serious infections, including life-threatening infections and death, have happened in people taking ARCALYST. Taking ARCALYST can make you more likely to get infections, including life-threatening serious infections, or may make any infection that you have worse.
- Risk of Cancer. Medicines that affect the immune system may increase the risk of getting cancer.
- Allergic Reaction. Stop taking or giving ARCALYST and call the healthcare provider or get emergency care right away if you get any of the following symptoms of an allergic reaction while taking ARCALYST:
- Rash
- Swollen face
- Trouble breathing
- Changes in your blood cholesterol and triglycerides (lipids). Your healthcare provider will do blood tests to check for these changes.
Common side effects:
- In people with CAPS and RP, the most common side effects of ARCALYST include:
- Injection-site reactions including: pain, redness, swelling, itching, bruising, lumps, inflammation, skin rash, blisters, warmth, and bleeding at the injection site.
- Upper respiratory tract infections
- Joint and muscle aches in RP
- In people with DIRA, the most common side effects of ARCALYST include:
- Upper respiratory tract infections
- Rash
- Ear infection
- Sore throat
- Runny nose
These are not all the possible side effects of ARCALYST. Tell your healthcare provider if you have any side effect that bothers you or does not go away. For more information, ask your healthcare provider or pharmacist.
The Kiniksa OneConnect™ program is made up of a team of dedicated Patient Access Leads who provide personalized one-on-one support at each step of your treatment journey with ARCALYST. You can find services to help you with starting treatment, financial assistance, and treatment support. You can contact a Kiniksa OneConnect™ team member at 1-833-KINIKSA (1-833-546-4572) Monday-Friday (8 AM – 8 PM ET).
Your Kiniksa OneConnect™ Patient Access Lead will help you coordinate the delivery of your medication and supplies.
ARCALYST Clinical Educators are qualified personnel who can assist you with virtual or in-person training to help you better understand the self-injection process.
Your first dose of ARCALYST (referred to as the loading dose) will be given as 2 injections of ARCALYST with the help of a healthcare provider in their office or with support from an ARCALYST Clinical Educator.
The loading dose is twice the dose of the following, once-weekly “maintenance doses” that you will prepare and self-administer.
SC, subcutaneous.
Take ARCALYST exactly as prescribed by your healthcare provider.
ARCALYST is given by injection under the skin (subcutaneous injection) 1 time each week. A healthcare provider will tell you how much ARCALYST to take. The Kiniksa OneConnect™ program can work with you to set up one-on-one injection training sessions with an ARCALYST Clinical Educator, so you are familiar with the administration process. Do not try to give yourself ARCALYST injections until you are sure that you understand how to prepare and inject your dose. Call your healthcare provider, pharmacist, or your Kiniksa OneConnect™ Patient Access Lead at 1-833-KINIKSA (1-833-546-4572) if you have any questions.
Other resources include the Step-by-Step Injection video, the Step-by-Step Injection manual and the ARCALYST Instructions for Use.
ARCALYST is a once-weekly, self-administered medication given by injection under the skin (subcutaneous).
Keep ARCALYST in the carton it comes in to protect it from light. Store ARCALYST in the refrigerator between 36 °F and 46 °F (2 °C and 8 °C). Refrigerated ARCALYST can be used until the expiration date printed on the vial and carton. ARCALYST may be kept at room temperature after mixing with sterile water for injection and should be used within 3 hours of mixing.
Keep ARCALYST away from light, and keep ARCALYST, injection supplies, and all other medicines out of the reach of children.
If you miss a dose, you should speak with your healthcare provider.
For more information, please see the full Prescribing Information.
It is normal for the powder in the ARCALYST vial to appear as a solid clump or disc. If this is observed, continue following the steps related to the reconstitution of ARCALYST as outlined in the Instructions for Use. You may need to shake the vial back and forth for an extended period of time (repeat step 25 in the Instructions for Use) until the powder has completely dissolved and the solution is clear.
ARCALYST should be stored in the refrigerator between 36 °F and 46 °F (2 °C and 8 °C) until it is time to prepare the product for your dose.
If you receive your ARCALYST and the product feels warm to the touch or the temperature monitor inside the shipping container has been activated, please contact your Patient Access Lead who can provide guidance on the use of the product.
Talk to your healthcare provider if you experience any side effects that bother you or that do not go away. Please report side effects by contacting Kiniksa Pharmaceuticals toll-free at 1-833-546-4572, Option 3, or contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Active ingredient: rilonacept.
Inactive ingredients: glycine, histidine, L-arginine, polyethylene glycol 3350, and sucrose.
connect with advocacy and support groups
As awareness of pericarditis, including recurrent pericarditis, grows, so does the number of groups and websites that support the pericarditis community. For information about recurrent pericarditis, please see these organizations. The organizations listed here support various conditions, including recurrent pericarditis.
While Kiniksa may provide funding to one or more of these institutions, Kiniksa neither endorses nor is responsible for the content of any of these listed websites or the services provided by these organizations.

The Pericarditis Alliance is dedicated to the management and treatment of pericardial disease through research, education, and support for patients and healthcare providers.
Learn More
The Myocarditis Foundation provides resources for patients, their families, healthcare professionals, and researchers about myocarditis and pericarditis.
Learn More
The American Heart Association is a relentless force for a world of longer, healthier lives. It funds innovative research, advocates for the public’s health and shares lifesaving resources.
Learn More
NORD is a patient advocacy organization dedicated to individuals with rare diseases and the organizations that serve them.
Learn More



