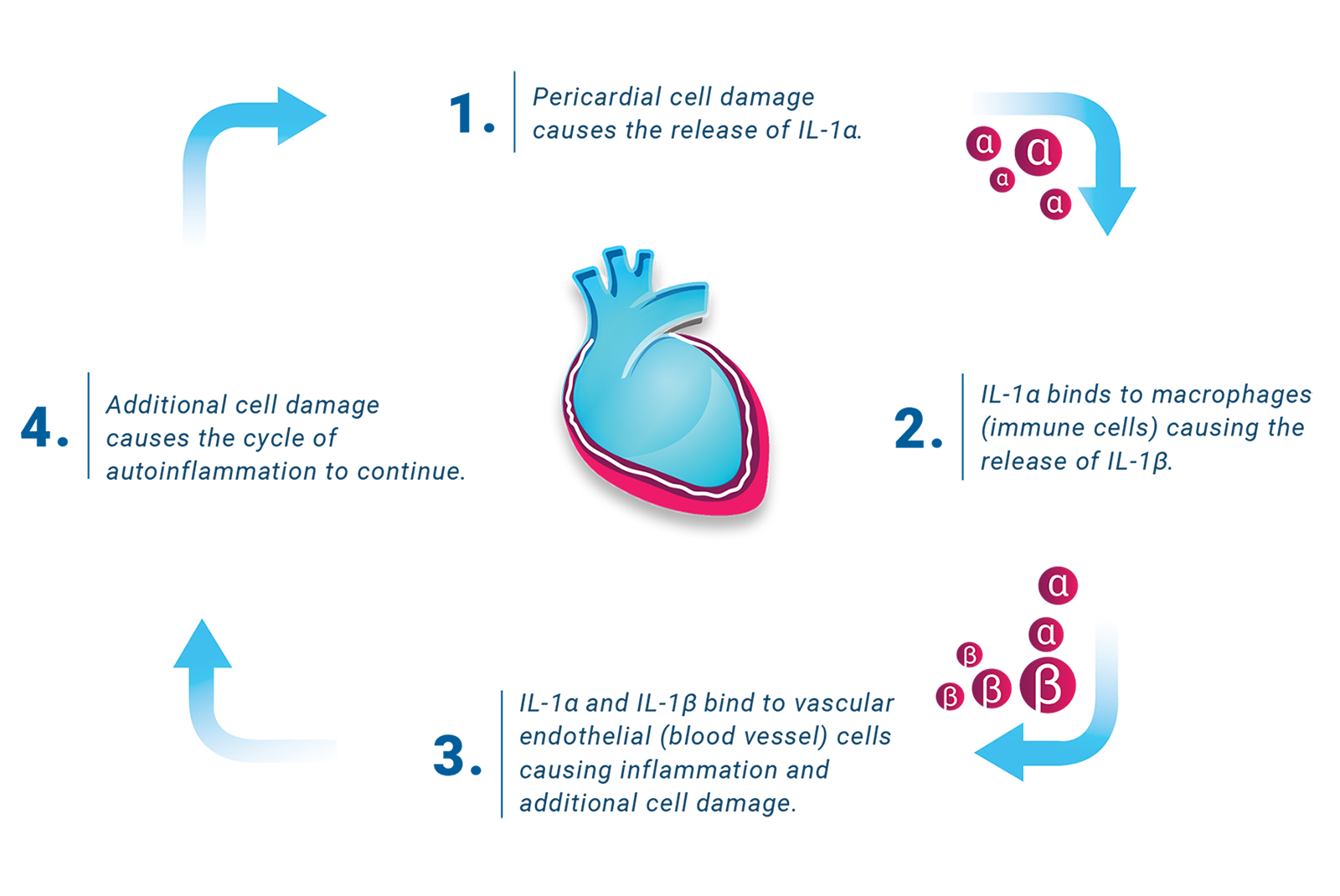
Traditional therapies—such as nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, and corticosteroids—are often used to manage symptoms of a first episode of pericarditis. Treatment for recurrent pericarditis needs a different approach because traditional therapies do not specifically target the ongoing cycle of autoinflammation that causes recurrent pericarditis.
Long-term prevention of flares requires a treatment that can break the cycle of autoinflammation.